The Battle Against Pneumonia
16 days.
That's the number of days Leon stayed in the hospital. If we're Facebook or Instagram friends, you probably know the story behind Leon's misdiagnosis which eventually led us to hospital confinement due to pneumonia. To make the long story short, after seeing 2 General Practitioners and 2 emergency doctors, we were told that Leon's spiking temperature, chills and vomitting were all caused by a viral infection - enterovirus, as confirmed by a swab test the GP did. We were advised to rest, drink plenty of fluids and administer fever-reducing medicine at home to fight-off the said virus.
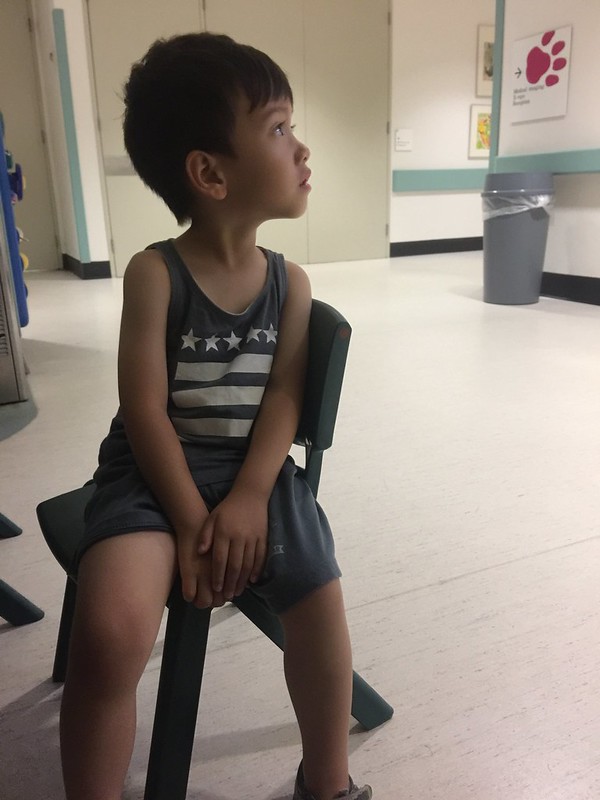
Leon while being rushed to the Auburn Hospital Emergency Department
The last GP we saw advised us to rush Leon to the Westmead Children's Hospital if he is still febrile on the 5th day of illness. That morning of Sunday, November 5, once the thermometer read 38, we immediately rushed him to the Kids Hospital. At the emergency department, he was thoroughly checked, his chest x-ray was taken and the next thing we know, we are being transferred to Hunter Bailey Ward cause Leon has pneumonia on his lower right lung.
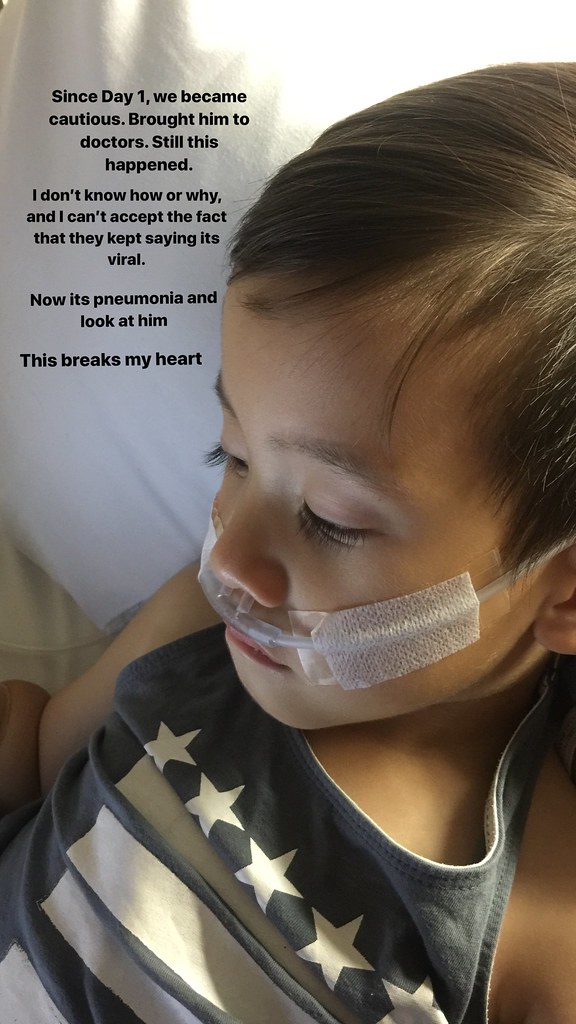
In the Westmead Kids' ER
Initially, we are referred to a team of a pediatrician. Leon was initially prescribed with intravenous antibiotics - Penicillin for 3x a day. We expected that in 3-5 days, Leon would respond to antibiotic treatment, and everything shall pass. However, we were wrong. I had a feeling that his pneumonia was bad when he needed to have an oxygen support of 0.5lpm (litres per minute) to support his breathing later that day.
Monday afternoon things spiraled down. Leon's temperature spiked high to 39.8, his heart rate went up to 170bpm and his breathing was really labored. Our nurse, Ate Mads, a Filipina, fortunately, called a rapid response to re-evaluate Leon's status. Right then and there, the doctors, the nurses and team leaders had an exchange of thoughts on how to manage Leon's condition. While the pedia team insisted that no ultrasound was needed and the antibiotic can work its way, the ICU nurses and Ate Mads insisted otherwise. In a flick of an eye, we found ourselves being transported to the ultrasound room. Our case was immediately transferred to the respiratory team as the scan confirmed a moderate (effusion) amount of fluid sitting on his right lung. They changed his antibiotics, increased his oxygen support to 1 litre and prepared us for a possible pleural drain for the next day.
The doctors explained that a pleural drain involves inserting a small tube on the side of his right chest to suck the fluid out of his lung. Initially, the surgery team declined to do the procedure for they believe that the effusion fluid in the lung is too small to be operated on. Somehow, Paolo and I were relieved, cause as much as possible, we would like to avoid any invasive procedure to be done to him.
After Leon's pleural drain insertion
However, the respiratory team was not comfortable with that decision. They referred our case to the interventional radiology, who then agreed to perform the insertion of the drain. With a heavy, worried and anxious hearts, we agreed on the treatment. I even brought him to the anesthesia room and help the doctors administer the anesthesia on him. You don't know how heartbreaking it is to comfort your son as he tries to resist all the doctors who touch him. I had no choice but to be strong.
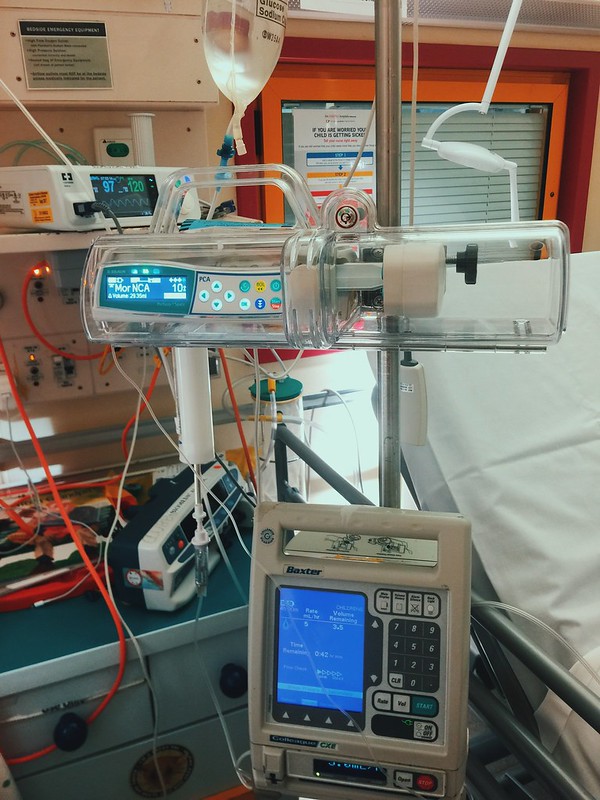
Morphine for his pain relief
The procedure lasted for at least an hour. Leon was fuzzy and restless in the recovery room that Paolo and I had to help the nurse in securing all his tubes - the oxygen, the drain, the PICC line and many more. Never in our lives, we imagined that we will witness our son undergo such procedure in an early age. Nakakatakot, nakakakaba.
Daddy gave him this mini-cooper the day after the first procedure to make him feel better.
To relieve his pain, a dose of morphine was given to him. To help melt all the gunk inside his chest, a medicine, called urokinase was administered in the drain Ideally, after 4 hours, this medicine will help flush the fluids out and remove all the fluids from inside his lungs. While the first dose was successful, the second dose of the urokinase did not drain any more fluids. Leon's temperature was still spiking high, his heart rate was still high and his breathing was still labored. His oxygen requirement even went high up to 2 litres per minute. 2 days after his first pleural drain, Leon's physical symptoms did not improve. His drain is not draining any fluids., Then, his condition had to be re-evaluated. After another round of chest X-ray and ultrasound, doctors found out that the fluid inside his lungs moved to a different position - to a position where the drains could not reach.
Leon at the recovery room after the VATS procedure
How 2nd the chest drains looked like. 2 tubes were inserted 1 hole to get all the fluid in the lungs.
Come Friday, 3 days after the pleural drain insertion, the surgical team then took over Leon's case. Instead of repositioning the drain, the doctors decided to mechanically remove the fluid and the gunk through a procedure called VATS Video-assisted thoracoscopic surgery. From a small hole in the lungs, the surgeon used a camera to help perform the procedure. For 4 scary hours, Leon was in the theatre, having his lungs operated on while Paolo and I anxiously waited outside.
I remember crying so hard in the parents lounge. Nangangatog ako sa kaba. Waiting was the hardest part. Lahat na yata ng bagay naisip ko. Lahat na yata ng santo, nadasalan ko. I never expected that Leon's pneumonia was that complicated that a second procedure was necessary to cure him. However, all my worries, my paranoia has passed when we were called by the doctor to see him in recovery.
Leon 2 days after the VATS - trying to stand up. See his tubes at the back.
This time, Leon was settled and fast asleep. Another drain was placed on his back, this time to collect any remaining fluid on the lungs. The surgeons showed us the x-ray right after the procedure and we saw the significant improvement in his right lung. After they removed all the fluid and all the nasty mucus inside, halos nagclear up na yung lungs. We were so optimistic this time. Finally, we can finally claim that Leon is indeed on his way to recovery.
However, as like any other roads, the road to recovery was very very bumpy. The next day, Saturday, the doctors and nurses saw that Leon has a worrying edema. Sobrang manas na nya, nakakatakot na. So, they transfused an albumin - they say that the drain and the infection can decrease the level of albumin, the protein responsible in absorbing the fluid in the blood vessel. With blood levels confirming a very low amount of albumin, they gave him albumin. They also gave a couple of doses of medicine to make him pee (I forgot the name of the medicine) to relieve his edema.
Leon hugging the stuffed toy given my workmates
Tuesday, more than a couple of days after I noticed that Leon was still peeing excessively. I reported it to the doctors and the nurses who told me that it is still normal. Yet, my instincts say otherwise. Later that night, I reported to the nurse that I am really bothered. Leon looked really thin. He is on 5ml/hour rate on dextrose and his fluid intake is still not much, but he keeps on wetting the bed. I told the nurse, my son needs to be hydrated to help him recuperate. 3 days post-op his temperature still spikes up to 39. Dahil sa kakulitan ko, nagpaclinical review si nurse. Gladly, they were weighing the nappies and the doctors found out na he was already -600mls dehydrated. Immediately, they increased his fluids to 50ml/hour.
Celebrating Paolo's birthday and our 4th year wedding anniversary in the hospital
The next day, Wednesday the surgeons finally pulled out the drain. They also removed the oxygen support which means his lungs are now getting back to normal. I was in the treatment room when the anesthesiologist administered laughing gas on him. Ang hirap pa-kalmahin si Leon. Ang sakit sa puso pero wala naman akong choice. Anyway, while I thought recovery is finally on its way, we experienced another setback. Four hours after it was removed, Leon's drain site was bleeding. When I called the nurse, immediately, a rapid response was made. Hindi ko inexpect na big deal pala yung pagkaka-alis ng dressing nya. All the nurses were putting pressure on his back while they were waiting for the doctors. Leon was crying hysterically. Ang sakit siguro hawakan at tuunan ang surgery site mo nang walang pain relief diba?
Moments after the drain was removed. Look at the effect of the laughing gas!
We gave him a dose of pain reliever - something similar to morphine while everything was happening. For half an hour, the doctors and the ICU nurses re-dress the site in a way that it will not fall off again. The xray was done on the spot and it confirms the absence of pneumothorax. If Leon's dressing was not immediately actioned, air might come inside the lungs and will cause bigger problems. Buti nalang, naagapan. He was strictly monitored the following days because of what happened. Good thing, his stats were okay and his breathing did not changed. We only battled against an annoying concern - his fever.
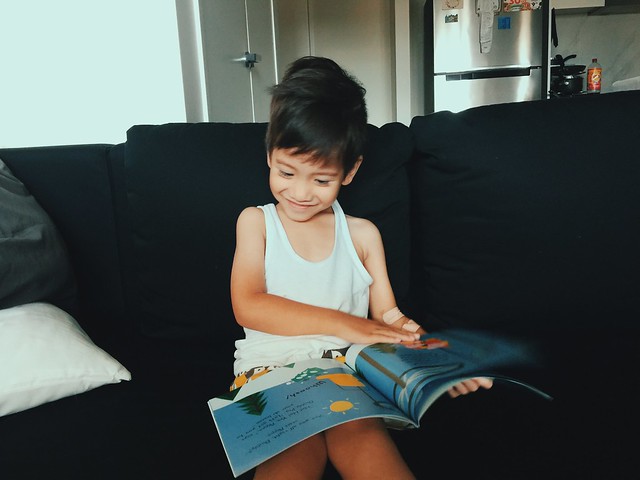
Leon, feeling much better on Day 13 in the hospital, except for the fevers
Despite being on 2 IV antibiotics (kepotaxime and clindamycin) for more than a week, his temperature still goes up to 39 degrees. While there are many reasons for his temp - it could be viral, it could be another infection, doctors say that it is still caused by his pneumonia. Without a full 24-48 hours of fever free, or at least low-grade fever (which is 37.6-38.4), we cannot go home.
Sunday, Day 15 when we went outside the ward to walk. His physiotherapists were impressed.
We were supposed to be discharged Monday, November 21 but was halted cause Leon's surgical site still has some air leakage. Ideally, 5 days from the time the drain was pulled out, the wound should be dry already. However, since Leon is very special, he belonged to that small percentage of patients whose site does not heal fast. Thus, we were asked to stay for one more night, until the surgeons fix a secure dressing, a dressing fit to be sent home.
The elves came to visit the sick kids and gave some presents. Leon felt so happy
Paddington!
Finally, after 16 days, Tuesday, we got the discharge notice. After the surgeons fixed the dressing, his x-ray confirms better lungs with no pneumothorax. We were advised to send him to GP after 5 days to have him checked, and to have his dressing cleaned. He was given iron supplements cause his hemoglobin dropped low. He was advised to eat well and regain the 2 kilos he has lost from the disease. He was also advised to stay at home for at least a week before he can finally to childcare.
Currently, we are very much relieved to finally be home. Slowly, Leon is getting back on his old, active, playful self. His appetite is getting huge and his energy is getting stronger each day. His physiotherapist advised us to make him move as much as possible, for better recovery and we are doing such. His dressing has a little puss and some air leak - but doctors say not to worry as long as its secured. Hopefully, come Monday he will be cleared and he can finally regain his (and our) "normal" life back.

















Comments